What is Vasectomy Reversal?
For many years, doctors have been helping male patients with a popular form of birth control, the vasectomy – a simple procedure whereby the tubes that carry sperm from the testes are cut and tied to stop the flow, preventing pregnancy.
Fortunately, for the many patients who change their mind about parenthood, the procedure can be reversed in one of two ways – by Vasovasostomy (vasectomy reversal) or Vasoepididymostomy (microsurgical vasectomy reversal).
Now, thanks to significant technological advances, NEW methods for vasectomy reversal have emerged using robotics. These ground-breaking procedures appear easier and safer than the long-standing traditional methods and better for the surgeon and the patient.
Just how effective is Robotic Vasectomy Reversal and does the procedure benefit male infertility treatment?
Initial Evaluation of Robotic Technology for Vasectomy Reversal
The complexities of traditional methods
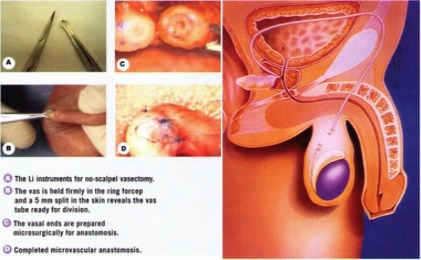
When it comes to vasectomy reversal, even the most experienced urologist can undergo strain and technical difficulty in this otherwise quick and painless procedure. This is mainly due to the vas deferens – the tubes that carry the sperm – being so small that the sutures (stitches) used to reconnect them are about the size of a human hair. While relatively simple to cut during a vasectomy, it is significantly harder to reattach them during a vasectomy reversal, and requires the surgeon to use a microscope for a close enough view of the structure. The high concentration and focus required to perform a vasectomy reversal is often interrupted when the surgeon needs to refocus the microscope or enter a new depth of field.
The new age of technology
Now, robotic systems are changing this process for the better. In Sydney, the new RoboticScope® high-definition digital imaging system – currently undergoing clinical trial at the San hospital – presents surgeons with a 30x magnified image of the vas deferens, removing the manual microscope used traditionally for vasectomy reversal. The revolutionary system includes a head-worn camera that projects a 3D image onto a screen, permitting the operating team to make crucial procedural decisions in real-time.

As such, this type of technology presents huge advances for microsurgical procedures, allowing surgeons to work ergonomically, using head movement to refocus and adjust depth of field while their hands prioritise their surgical technique. The strain and fatigue that often occur during a long, complicated surgery are reduced, and the surgeon can focus purely on the operation.
Microsurgical Robotic Assisted Vasovasostomy (RAVV)
The RAVV procedure follows the same principles as the traditional microsurgical vasovasostomy; the difference lies in the technology used for the operation and the benefits this delivers to both surgeon and patient.
Robotic Vasovasostomy Surgery Technique
The vas deferens walls are made up of several layers of tissues, primarily an inner and outer layer. Some surgeons choose to reconnect one layer – known as a single-layer vasovasostomy – while others will reconnect both layers. Either way, it is critical to connect both ends of the vas deferens properly so they heal fully and create a watertight seal, allowing the sperm to flow successfully out of the penis.
Before any surgery, a surgeon first assesses whether any sperm is present. This is done by cutting the vas deferens with a scalpel, creating two open tubes. If they detect sperm, there is a higher chance of fertility once the vas deferens are rejoined.
The patient lies horizontally alongside the robotic platform to complete the robot-assisted vasovasostomy. In place of a manual microscope, the robotic arm and camera allow the surgeon a microscopic view of the vas deferens, leaving their hands free to reconnect each of the tubes and apply the sutures timely and accurately. The procedure takes between 2-4 hours to complete, with the patient placed under general anaesthetic.
Advantages and Outcomes
The key advantages are mainly process-based, with the robotic component improving vision and precision for the surgeon and reducing complications caused by hand tremors. There is also less training involved than with microsurgical training, which means a faster time to the operating theatre for medical professionals and a greater ability to support a surgeon during the procedure.
In terms of outcomes, medical assessment to date shows the RAVV procedure results in similar patency rates as the traditional microsurgical approach.
Microsurgical Robotic Assisted Vasoepididymostomy (RAVE)
As is the case with RAVV, the traditional vasoepididymostomy procedure is also now available using robotics in place of a manually-held microscope to enhance the surgeon’s efficiency.
Robotic Vasoepididymostomy Surgery Technique
The purpose of a robotic vasectomy reversal is primarily to resume a patient’s fertility. While RAVV is the more likely of the two procedures, for some patients, it is not possible to perform a vasovasostomy and rejoin vas deferens to vas deferens for effective sperm flow. Typically, this is due to the epididymis (downstream pipe) having been damaged in some way, likely because the of the ageing process. In this case, a surgeon performs a vasoepididymostomy, connecting the vas deferens directly with the epididymis to facilitate the sperm flow from the testicles to the penis.
Surgeons can only determine whether a RAVE is required once they begin operating on a patient and see the seminal fluids. If there is no sperm or the seminal fluid is thick in consistency, they will override a proposed RAVV procedure and instead, perform a Robot-assisted Vasoepididymostomy, or RAVE.
Similar to the RAVV procedure, the technology used for RAVE surgery negates the need for a manual microscope, giving the surgeon more freedom to complete this intricate procedure ergonomically and with less chance of fatigue. Surgery takes place under a general anaesthetic and is completed in just 2-4 hours.
Advantages and Outcomes
The technical component of the RAVE procedure has multiple advantages for medical teams. With the manual handling of a microscope removed, surgeons can focus on the operation itself rather than constantly readjusting the view, reducing unnecessary complications and fatigue. Whole teams can view the procedure in real time and make recommendations to support the surgeon.
While initial results show the patency levels as similar to their non-robotic counterpart, they are certainly no less – cementing RAVE as an effective alternative to the traditional microsurgical approach.
Postoperative Care
As with any medical procedure, it’s essential to understand what comes next in terms of recovery and care. After undergoing RAVV or RAVE, patients can expect the following:

The medical team applies bandages to the incision site. Tight-fitting underwear is recommended to help prevent these from moving around.

Swelling is likely, which can be managed by ice packs for 1-2 days following surgery.

Soreness may continue for a number of days, which can be managed by taking over-the-counter medication. The stitches should dissolve in around a week.
Avoid water for the first couple of days post-operation. Patients may be advised to keep your incision covered for longer when taking a shower.

Limit activities likely to pull on the testicles or scrotum – sport, running and heavy lifting.

Most men are advised not to have sexual intercourse or ejaculate for several weeks after the operation.

Jobs requiring physical labour that strain the body are safer to avoid for a few weeks.
Pros and Cons of Robotic Vasectomy Reversal Surgery
RAVV and RAVE are still in their infancy, which means it could be some time before medical teams can fully appreciate the potential benefits of these technologies for vasectomy reversal.
That said, these technically advanced procedures certainly look to improve male infertility surgery in numerous ways, with more reported advantages than disadvantages:
RAVV
Pros
- Greater operative efficiency
- Reduced surgeon fatigue
- Improved ergonomics
- Less training/faster time to certification
Cons
- Potential for longer operation time due to the technical set-up
- Risk of complications (also apparent with MVV procedure)
RAVE
Pros
- Greater operative efficiency
- Reduced surgeon fatigue
- Improved ergonomics
- Less training/faster time to certification
Cons
- Potential for longer operation time due to the technical set-up
- Risk of complications (also apparent with MVE procedure)
To date, there is little evidence that suggests robotic methods are superior to those used traditionally, with studies showing similar patency rates. In addition, the recovery times appear to remain the same whether robotics are involved in the procedure or otherwise.
Interestingly, the same studies have shown a greater patency and sperm count in patients living with a vasectomy for over 20 years, and this alone presents a strong argument to use robotics moving forward.
As with any surgery, there are risks a patient must consider beforehand. While unlikely, vasectomy reversal can lead to complications such as infection at the incision site or bleeding in the scrotum. The choice to become a father might well outweigh any risks – but we urge anybody considering a reverse vasectomy to discuss all their options with a urologist.
Final Words
Emerging technologies present an opportunity to improve our current methods for vasectomy reversal, with higher accuracy and less fatigue for the surgeons performing these life-changing male infertility treatments.
Currently in their infancy, we can expect these procedures to increase in availability and become more mainstream in the next few years. As always, Dr Katelaris will continue to pioneer advanced and traditional urological methods to improve the quality of life for patients in Sydney.
Katelaris Urology is a leading urologist in Sydney with over 35 years of experience performing minimally invasive, no-scalpel technique vasectomies and vasectomy reversals.
Dr Katelaris recently performed the first robotic Vasectomy Reversal in Australia using the RoboticScope platform.
For information about this ground-breaking surgery or support with male health issues, arrange an appointment with a consultant at Katelaris Urology today.
References
Vasectomy reversal (2023) Mayo Clinic. Available at: https://www.mayoclinic.org/tests-procedures/vasectomy-reversal/about/pac-20384537#:~:text=Doctors%20performing%20this%20surgery%20usually,MOS%2Dtuh%2Dme). (Accessed: 04 September 2023).
Robot-assisted vasovasostomy and vasoepididymostomy: Current status and … Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7483453/ .
The Infectious Diseases Society of America guidelines on the diagnosis … Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7929045/ .
Revolutionising the world of microsurgery RoboticScope. Available at: https://www.bhs-technologies.com/wp-content/uploads/2021/12/BHS_Broschuere-A4-download.pdf .