What is Prostate Cancer?
It is likely you have heard of Prostate Cancer already. It’s the second-most diagnosed type of cancer in Australia today behind skin cancer. In 2022, over 24,000 Australians were diagnosed as positive* – 1.4 million globally – helping it rank in the top 2 cancer types throughout the world.**
But what is prostate cancer?
The prostate is a small gland found in the male body, and holds the seminal fluid responsible for transporting sperm. Like most of the human body, it is made from cells. When those cells grow out of control and become abnormal, cancer develops.
In its simplest terms, prostate cancer is classified as either early or late stage. Early-stage prostate cancer means the cells have grown but remain within the prostate gland. Late-stage prostate cancer means the cancer has spread beyond the gland to other parts of the body, making it more difficult to treat.
Like with many cancers, early detection is key to giving diagnosed patients a much higher chance of a permanent cure. Unfortunately, it can quickly become aggressive where left undetected and much tougher to cure altogether – but it can be managed, thanks to modern methods introduced in recent years.
Here is everything you need to know about Prostate Cancer, including Diagnosis & Screening, Treatments and Rehabilitation.
About Prostate Cancer
Prostate Cancer Causes
While the cause of prostate cancer is not clear, research has uncovered a series of commonalities between diagnosed males from around the world to help us understand the potential causes.
Strong evidence suggests men who are overweight, obese or tall in height are at most risk. Family history is also important, with men much more likely to receive a diagnosis if their father or brother has received one, or their mother had breast cancer.
Other less common factors in men diagnosed with prostate cancer include those with a high dairy consumption, plus a diet high in calcium and vitamin E.
Prostate Cancer Symptoms
As with all cancer types, the symptoms will vary from one person to the next. Worryingly, when prostate cancer remains in its early stages, there could be no symptoms whatsoever, leaving it to go overlooked.
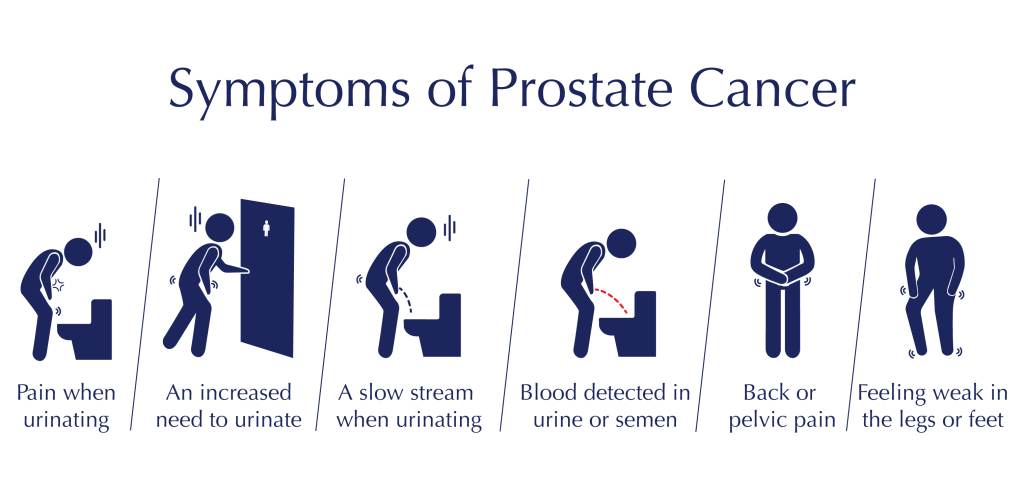
Once the cancer has progressed, a number of symptoms will emerge in most men, including one or more of the following:
Bear in mind these symptoms may point towards another health issue. Yet if you are experiencing any such symptoms, it is advised to book an appointment for a prostate screening test as soon as possible.
Prostate Cancer Diagnosis & Screening
According to current data from the Australian Cancer Research Foundation, 1 in 5 men in Australia will be diagnosed with prostate cancer before they turn 85**. The average age when diagnosed is 69.
As you will appreciate, with numbers this high, regular screening for prostate cancer is imperative – whether you are experiencing symptoms or not.
In Australia, males are encouraged to book a prostate check with a Urologist once they reach the age of 50, and to continue doing so at two year intervals. Or, if a family member has already been diagnosed with prostate cancer, medical advice suggests men arrange their first screening test between the ages of 40 and 45.
Remember: early diagnosis always presents the best chances of a cure.

PSA testing
Prostate-Specific Antigen (PSA) blood testing assesses the prostate cells for normal and abnormal behaviour. It is not a definitive test – some men with an abnormal PSA level still won’t develop cancer. This serves as a starting point only and requires further testing to determine whether cancer is present.

Genomic testing
The Oncotype DX prostate cancer test helps determine when cancer is present and how aggressive it is, helping medical teams to guide their patients on suitable treatments.
The test begins with a biopsy, with the genes taken in the sample analysed create a Genomic Prostate Score. It predicts the likely biological behaviour of the cancer cells and how they will progress over time, helping a urologist determine whether treatment will benefit the patient.

Prostate MRI scan and prostate biopsy
Magnetic Resonance Imaging (MRI) technology is used by radiologists to scan body organs and look for defects. A prostate MRI scan shows the prostate and surrounding tissue in great detail, allowing for detection of tumours as small as 0.5ml, and high-grade prostate cancer that requires treatment.
If the MRI scan detects legions – which may or may not be cancerous – a biopsy is recommended. An MRI-guided biopsy has a high accuracy rate and reduces the need for multiple biopsies.
Prostate Cancer Treatments
In recent years, we have seen massive advancement in the treatments for prostate cancer, some of which capable of removing the cancer completely.
The most suitable course of prostate cancer treatment depends on the severity. For example, low-grade prostate cancer requires monitoring in place of an aggressive treatment.
Here are the main types of prostate cancer treatment currently available:
Radical Prostatectomy
This treatment type is a major surgical procedure. Developed in 1982 by Professor Patrick Walsh, the term ‘radical’ refers to its nature, which involves the complete removal of the prostate, seminal vesicles and associated pelvic lymph nodes. Forty years on, it remains the leading treatment for men with localised prostate cancer.
While Radical Prostatectomy has a high level of success, there are a number of side effects to make patients aware of, the most common ones being incontinence and erectile dysfunction. All considerations are discussed between patient and urologist to help determine the right course of treatment.
Active surveillance
As it might sound, this is not a ‘treatment’ as such, and involves regular monitoring of the prostate to check its current condition. It is a common course of action recommended for men with low grade prostate cancer, who are not yet at a stage where aggressive treatment is necessary. That said, prostate cancer is a serious condition whatever its stage, and regular on-going monitoring means both the patient and their medical team keep across changes to the cancer as and when they occur.
Radiotherapy
For some patients where a Prostatectomy isn’t possible – the cancer has spread beyond the prostate, for example – radiotherapy presents a viable treatment option. In this scenario, a radiation oncology specialist can administer External Beam Radiation Therapy (EBRT) or by implanting radioactive seeds (Brachytherapy).
Advanced Therapy
Endocrine therapy is a hormones treatment, reducing the amount of testosterone to slow down the cancer growth. It is used only for patients with advanced prostate cancer, and comes with a number of known side effects including impotence, osteoporosis and heart problems. If and when a patient has exhausted hormone therapy, they might be offered chemotherapy. A highly aggressive treatment, the chances of negative side effects become greater still – hair loss, nausea, bone marrow suppression and nerve damage among them.
Treatment Options by Stage
Every prostate cancer diagnosis – early or late – is given a stage to further classify the severity.
Prostate cancer stages are calculated by the level of Prostate-Specific Antigen – or PSA – found in the blood. Once the cancer stage is known, it allows medical staff to advise a patient on the most suitable types of treatment available.
Stage I Prostate Cancer
At this stage, prostate cancer is still termed as ‘localised’ – it is in its early stage and only in the prostate. The detected cancer is found in half of one-side of the prostate and is considered a low threat.
Stage II Prostate Cancer
This stage of prostate cancer has progressed further and while still localised (confined to the prostate), it may spread. There are 3 sub-stages – A, B and C – with Stage IIA showing cancer in one side of the prostate and Stage IIC in both sides.
Stage III Prostate Cancer
When prostate cancer reaches this stage, PSA levels are high and the cancer has spread to tissues beyond the prostate. It is termed a high grade, locally advanced cancer.
Further classifications A, B and C help give more detail to the patient and medical teams about the risk and the advised treatments.
Stage IV Prostate Cancer
Stage 4 is the most aggressive prostate cancer – also called Metastatic – and has 2 sub classifications: ‘A’ means the cancer has spread beyond the prostate to the lymph nodes, and ‘B’ means the cancer has reached lymph nodes, bones or elsewhere in the body.
Early stage treatments include active surveillance, prostatectomy, and radiation therapy. Late stage treatments include prostatectomy, radiation therapy and advanced therapy.
Other Considerations
The primary objective for a patient and their medical team is to cure the body of cancer cells. Yet it is the responsibility of a urologist to provide as much information as possible to their patient about suitable treatments, including other considerations such as potential side effects.
After Prostate Cancer
There are two common side effects that can occur after aggressive treatment for prostate cancer:

Urinary Control
After undergoing a Prostatectomy, some patients suffer from urinary incontinence which is both inconvenient and embarrassing. Pelvic floor exercises are a good way to overcome urinary incontinence, and helps most men to recover within six months of their surgery. For those who continue with incontinence, elderly males in particular, methods for management include the Artificial Urinary Sphincter and the Sling Procedure.

Erectile Dysfunction
Unfortunately, this is a common after-effect of prostate cancer and not surprisingly, one which concerns most patients. Of course, it is not that prostate cancer itself causing a sexual dysfunction but a side effect of the treatment received by the patient – a Radical Prostatectomy or radiotherapy, specifically.Nowadays, sexual dysfunction treatments are more readily available to support any patients affected by their cancer treatment. One of the preferred treatments available is an injection, which is effective when administered within 6 weeks of the cancer treatment.
Prostate Cancer Rehabilitation
Just as treatments have advanced in recent years, the mortality rates for prostate cancer have decreased, which is great news. Of course, curing patients is a priority but quality of life after cancer treatment is just as important, and men are encouraged to pursue a full rehabilitation programme to ensure the best possible outcomes for their physical and mental health.
FAQs
Can Prostate Cancer be cured permanently?
Like many cancers, prostate cancer stands its best chance of being cured if diagnosed early. In its initial stages, treatment can be successful particularly when the cancer is confined to the prostate and has not spread elsewhere in the body. Once it develops into late-stage prostate cancer, it can only be managed rather than cured, using medication such as Abiraterone or Enzalutamide.
What are the early signs of Prostate Cancer?
Unfortunately, prostate cancer often arrives without any symptoms. However, there are several commonalities between men diagnosed with prostate cancer which put other men in these categories at a higher risk than others:
There are other factors to consider including general health. Eating a balanced diet, exercising and keeping alcohol to a minimum all promote a healthy life.
- Men who have a family history of prostate cancer
- Men who are overweight or obese are more likely to contract prostate cancer
- Men with a rising PSA level
There are other factors to consider including general health. Eating a balanced diet, exercising and keeping alcohol to a minimum all promote a healthy life.
What is the safest way to treat Prostate Cancer?
Nowadays, there are multiple prostate cancer treatments available, all suited to the different stages of the disease. If you have been diagnosed with prostate cancer, it is advised to book an appointment with a urologist and discuss the best type of treatment suited to your stage of cancer, to help you remove or manage it.
What is the life expectancy of a man with prostate cancer?
While it is the second-most common cancer in Australia, there is currently a high survival rate for men with prostate cancer. Low-grade prostate cancer is manageable, with most men able to continue as usual while monitoring the cancer’s progress. High-grade prostate cancer requires intense treatment – likely, prostate surgery or chemotherapy – with a 96% chance of survival for five years.***
Who is most likely to get prostate cancer?
Prostate cancer is more likely to occur in older men aged 65 years and over. It is rare in men aged under 40 years, although it can happen. Family history puts men at a higher risk of diagnosis than others; men who are overweight are also more susceptible to prostate cancer.
What causes prostate cancer and how can it be prevented?
Several factors are said to increase the chances of a prostate cancer diagnosis. They include:
- A family history of prostate, breast or ovarian cancer (BRCA1 and BRCA2 gene mutations)
- A father or brother diagnosed with prostate cancer under the age of 60
- Age – with the risk increasing for men aged 50 years and over
While you cannot prevent prostate cancer, you can manage it by regularly monitoring the PSA levels in the blood. Men with an elevated PSA level do not always have cancer, and further tests are required.
What is the newest treatment for prostate cancer?
Treatments for prostate cancer differ depending on its stage. Surgery and radiation therapy are still the preferred treatments for patients with cancer confined to the prostate (localised).
Metastatic prostate cancer – when cancer has spread beyond the prostate – requires advanced treatment, such as hormone therapy or chemotherapy.
Research into prostate cancer is continuous as scientists search for new treatments that deliver a higher life expectancy.
What are the prostate cancer survival rates?
In Australia, the survival rates for men with prostate cancer remain high. Early diagnosis is essential to treating and curing the cancer; once it has progressed to high-grade prostate cancer, patients rely on a more intense course of treatment to remove or manage it. Currently, there is a 96% chance of surviving cancer for at least five years.
References
* Cancer Council
https://www.cancer.org.au/cancer-information/types-of-cancer/prostate-cancer
** World Cancer Research Fund
Cancer Australia (2019) Prostate cancer in Australia statistics, in Australia statistics | Cancer Australia. Available at: https://www.canceraustralia.gov.au/cancer-types/prostate-cancer/statistics#:~:text=Between%201989%E2%80%931993%20and%202014,from%2063%25%20to%2096%25


